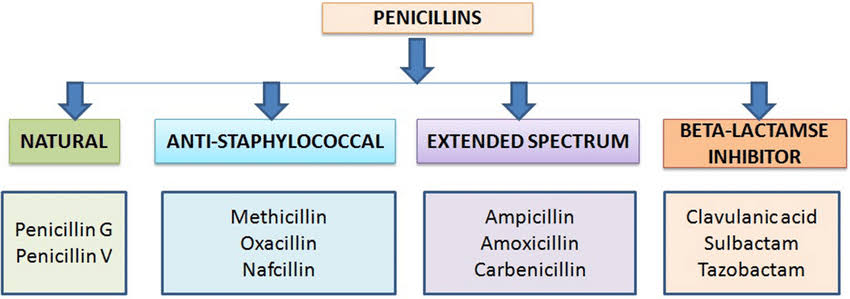
Penicillin, one of the most well-known and widely used antibiotics in the world, has evolved into a broad category of medications used to treat bacterial infections. Though originally discovered in 1928 by Alexander Fleming, penicillin has since been modified and adapted into various forms to better combat bacterial resistance and target specific types of bacteria. Among these variations, penicillins are typically categorized into four main types based on their chemical structure, spectrum of activity, and resistance to bacterial beta-lactamases (enzymes produced by bacteria that can break down penicillin). The four primary types of penicillin are:
- Natural Penicillins
- Aminopenicillins
- Penicillinase-resistant Penicillins
- Extended-Spectrum Penicillins (Antipseudomonal Penicillins)
This essay explores each type in detail, including their characteristics, common uses, and examples.
- Natural Penicillins
Natural penicillins are the original penicillin compounds derived directly from the Penicillium mold. These were among the first antibiotics to be used clinically and remain important in the treatment of various bacterial infections, particularly those caused by gram-positive bacteria.
Characteristics
Natural penicillins are most effective against gram-positive cocci, such as Streptococcus pneumoniae, Streptococcus pyogenes, and some Staphylococcus species (though many staph species are now resistant). They also target some gram-negative cocci like Neisseria meningitidis and spirochetes such as Treponema pallidum, the causative agent of syphilis.
These penicillins are susceptible to degradation by beta-lactamase enzymes, which limits their effectiveness against many modern bacterial strains that have developed resistance.
Examples
Penicillin G (benzylpenicillin): Usually administered intravenously or intramuscularly due to poor oral absorption. It’s used for treating serious infections such as syphilis, endocarditis, and meningitis.
Penicillin V (phenoxymethylpenicillin): Orally bioavailable and used to treat less severe infections like strep throat or mild skin infections.
Clinical Uses
Streptococcal infections
Syphilis
Meningitis (from susceptible strains)
Diphtheria
Actinomycosis
Despite their narrow spectrum and vulnerability to beta-lactamases, natural penicillins are still valuable for treating infections where susceptibility is known.
- Aminopenicillins
Aminopenicillins are modified penicillins that have an extended spectrum of activity compared to natural penicillins. They retain the core beta-lactam ring structure but include an amino group, which allows them to penetrate the outer membrane of some gram-negative bacteria.
Characteristics
These drugs have improved activity against certain gram-negative bacteria such as Escherichia coli, Proteus mirabilis, Haemophilus influenzae, and Salmonella species. However, like natural penicillins, they are still vulnerable to beta-lactamase enzymes, limiting their use unless combined with beta-lactamase inhibitors.
Examples
Amoxicillin: Often preferred due to better oral absorption and fewer gastrointestinal side effects compared to other aminopenicillins. Commonly prescribed for ear infections, sinusitis, and respiratory infections.
Ampicillin: Used for similar infections but often given intravenously in hospital settings. It’s also a treatment for infections like Listeria monocytogenes meningitis and enterococcal infections.
These antibiotics are often combined with beta-lactamase inhibitors to broaden their effectiveness:
Amoxicillin + Clavulanic Acid (Augmentin)
Ampicillin + Sulbactam (Unasyn)
Clinical Uses
Otitis media
Sinusitis
Urinary tract infections (UTIs)
Respiratory infections (e.g., bronchitis, pneumonia)
Bacterial meningitis (from Listeria or H. influenzae)
Endocarditis (caused by Enterococcus)
- Penicillinase-Resistant Penicillins (Anti-Staphylococcal Penicillins)
As bacterial resistance to penicillin became more prevalent—particularly in Staphylococcus aureus—a new class of penicillins was developed that could resist destruction by the beta-lactamase enzyme known as penicillinase.
Characteristics
Penicillinase-resistant penicillins are designed to be stable against beta-lactamase enzymes produced by Staphylococcus aureus. These antibiotics are mainly effective against gram-positive bacteria and are not useful against gram-negative organisms due to limited activity and inability to penetrate their outer membranes.
Examples
Nafcillin: Typically given intravenously for systemic infections.
Oxacillin: Similar to nafcillin, often used in hospitals.
Dicloxacillin: Orally active and used for less severe staphylococcal infections.
These antibiotics are particularly valuable in treating infections caused by methicillin-sensitive Staphylococcus aureus (MSSA), but they are ineffective against MRSA (methicillin-resistant Staphylococcus aureus).
Clinical Uses
Skin and soft tissue infections (e.g., cellulitis, abscesses)
Osteomyelitis
Endocarditis (caused by MSSA)
Septic arthritis
The use of these agents has become more focused as staphylococcal resistance patterns have changed, but they remain a cornerstone in treating susceptible staphylococcal infections.
- Extended-Spectrum Penicillins (Antipseudomonal Penicillins)
These penicillins have been developed to combat gram-negative bacteria that are resistant to other forms of penicillin. They are particularly important in hospital settings, where infections with difficult-to-treat pathogens like Pseudomonas aeruginosa are common.
Characteristics
Extended-spectrum penicillins have activity against many gram-negative organisms, including Pseudomonas, Enterobacter, and Klebsiella species. Like aminopenicillins, they are still susceptible to beta-lactamases and are often used in combination with inhibitors to enhance their efficacy.
Examples
Ticarcillin: Less commonly used now, but once widely employed in combination with clavulanic acid.
Piperacillin: The most commonly used antipseudomonal penicillin, often combined with tazobactam (as in Zosyn).
Combination products:
Piperacillin + Tazobactam (Zosyn): This combination is a mainstay in the treatment of serious hospital-acquired infections, including pneumonia, intra-abdominal infections, and sepsis.
Clinical Uses
Hospital-acquired pneumonia
Sepsis
Intra-abdominal infections
Complicated UTIs
Infections caused by Pseudomonas aeruginosa
Febrile neutropenia
Because of their broad spectrum and ability to target difficult organisms, extended-spectrum penicillins are typically reserved for severe infections and use in critical care settings.
Summary Comparison Table
Penicillin Type Examples Spectrum Beta-Lactamase Resistance Common Uses
Natural Penicillins Penicillin G, Penicillin V Gram-positive, some gram-negative cocci No Strep infections, syphilis
Aminopenicillins Amoxicillin, Ampicillin Gram-positive, some gram-negative No (used with inhibitors) Otitis media, UTIs, respiratory infections
Penicillinase-Resistant Nafcillin, Oxacillin, Dicloxacillin Gram-positive (especially MSSA) Yes Skin infections, osteomyelitis
Extended-Spectrum Piperacillin, Ticarcillin Broad, including Pseudomonas No (used with inhibitors) Hospital-acquired infections
Conclusion
Penicillin and its derivatives remain a foundational part of modern antimicrobial therapy. The four main types—natural penicillins, aminopenicillins, penicillinase-resistant penicillins, and extended-spectrum penicillins—each serve unique roles in clinical medicine. Their use is guided by bacterial susceptibility, site of infection, and resistance patterns. In an age of increasing antibiotic resistance, the strategic and informed use of these penicillin types, often in combination with beta-lactamase inhibitors, remains essential for effective treatment and stewardship of these invaluable drugs.